Welcome to NJHIMA
Health Information Professionals Week, April 15 - 19, 2024
Visit AHIMA for More Information:
- Messages from AHIMA Leadership
- FAQ Guide
- Celebration Toolkit

Call for NJHIMA Board Nominations, 2024-2025 Term
Nominate Someone Here Today!

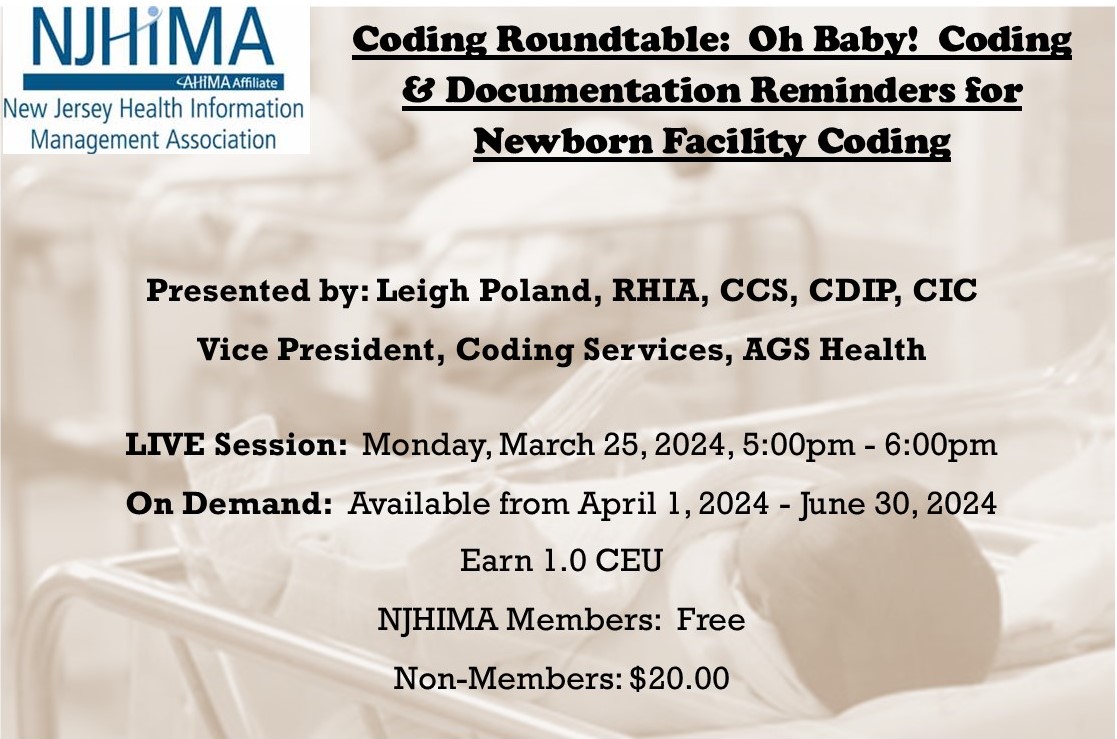
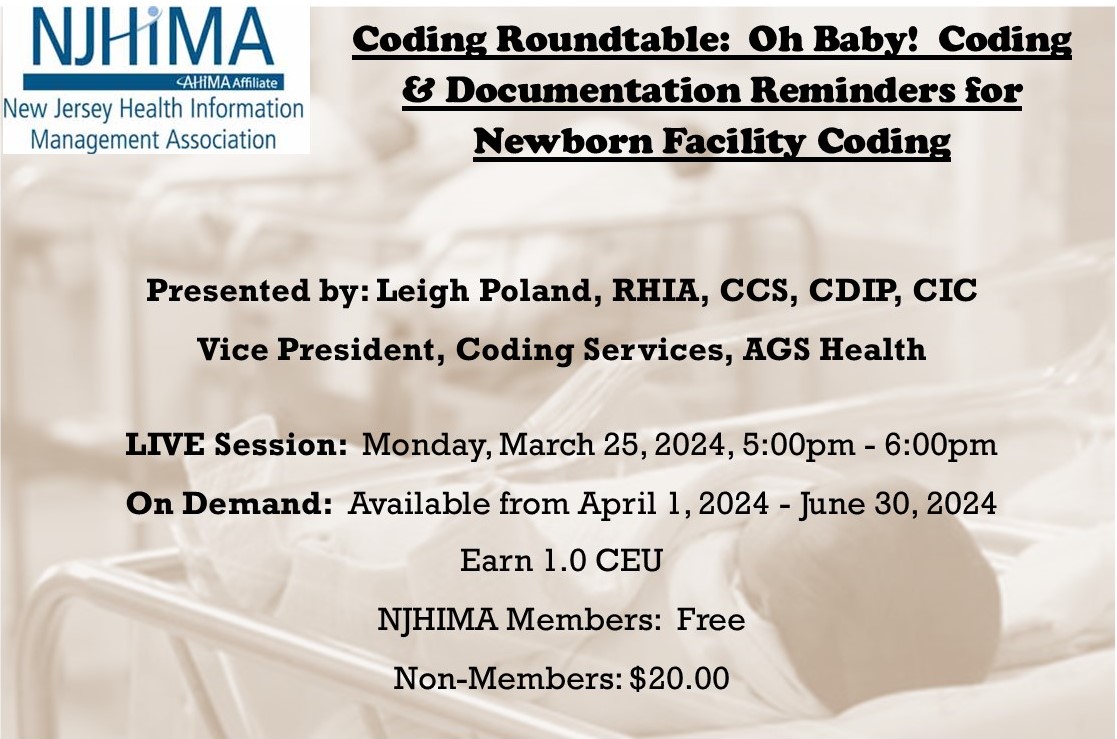
NOW AVAILABLE ON DEMAND!
Coding Roundtable: Newborn Facility Coding
Click HERE to Learn More & Register
New Jersey Authorization Legislation Recently Featured on STAT News
"Other states should follow New Jersey’s lead on prior authorization reform".
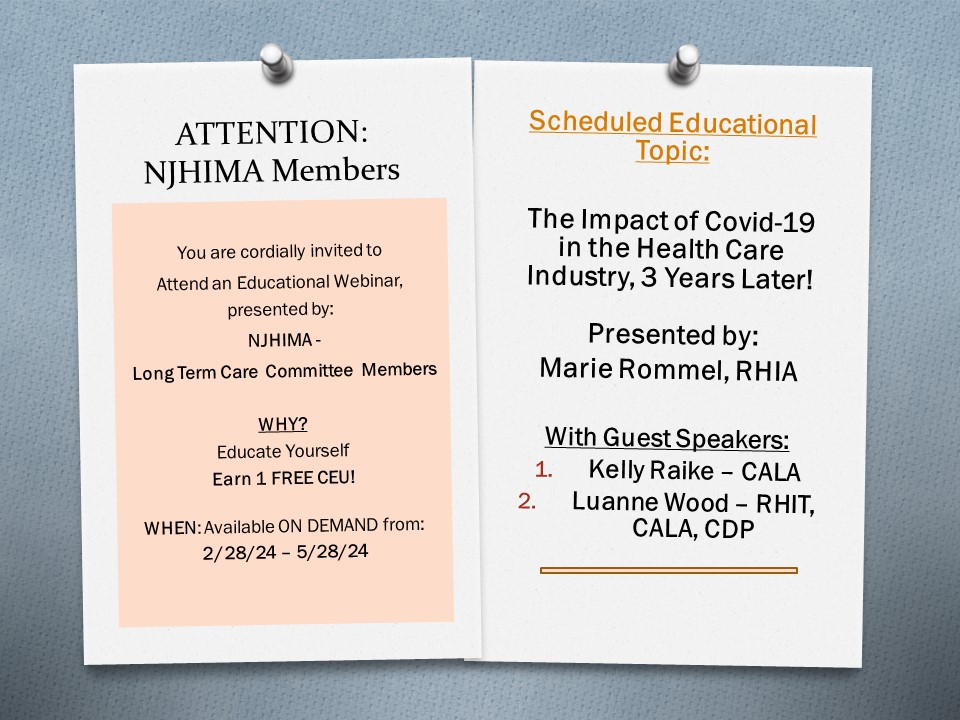
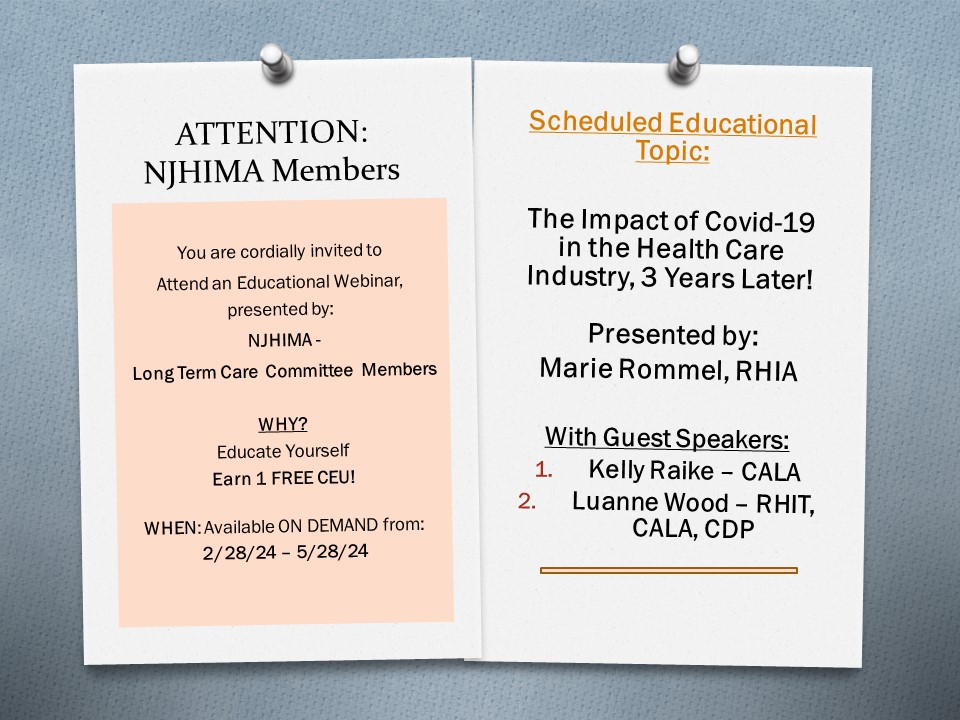
NEW! 2024 Long Term Care Quarterly Meeting
Open to NJHIMA Members ONLY*
Click HERE to Register NOW!
Note: Session is available to access on February 28, 2024
Education Corner
Latest News
|